Why Call Coverage Is a Flashpoint
This post is co-authored by Dennis Hursh, founder of Physician Agreements Health Law, and Rob Anderson, MD, co-founder of Marit Health. It combines Dennis’s experience advising physicians on employment contracts, Rob’s practical perspective as an anesthesiologist managing call, and Marit’s unique and comprehensive call data to provide a holistic view on call coverage terms and compensation.
For many physicians, call coverage is one of the most frustrating aspects of employment agreements. It disrupts rest, strains family time, and is often uncompensated. Yet hospitals frequently present call as a “given,” leaving doctors feeling as though they have little room to negotiate.
Too often, administrators respond to physicians’ concerns with generic explanations about “how the system works.” Attorney Dennis Hursh has described this dynamic as hospitalsplaining – when hospitals characterize physicians’ requests for fairer terms as naive, impractical, or out of step with reality.
The larger issue is not the language used in these conversations, but what it obscures: call expectations that are often unreasonable, with real consequences for physician well-being and, ultimately, patient care.
The Three Dimensions of Call
When it comes to call, three elements matter most:
- Frequency: How often call is required
- Location: Whether call is happening in-hospital or at-home
- Compensation: How much call is paid, if at all
In this post, we’ll focus on frequency and location. Next week, we’ll take a closer look at call compensation benchmarks.
Call frequency and location vary dramatically by specialty, so we developed a weighted score we’re calling the Call Burden Index to make it easier to do an apples-to-apples comparison across specialties. This index blends several factors:
- Percentage of physicians who report taking call
- Average number of call days per week
- Proportion of call happening in-hospital vs. at-home
Here’s the summary of call burden by specialty, sorted from highest burden to the lowest.
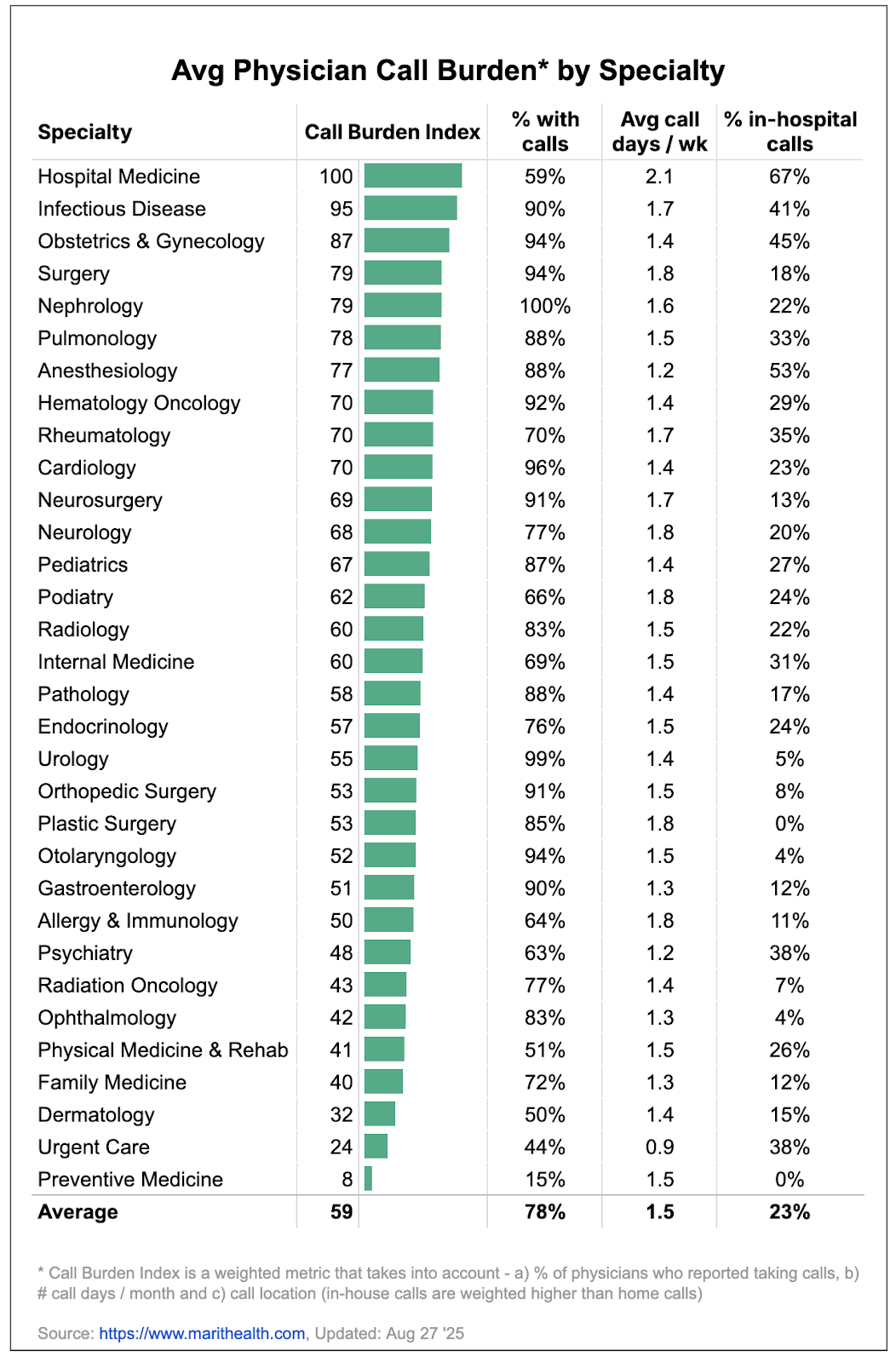
Hospitalists: 2.1 Call Days per Week, 67% In-Hospital
Even though only 59% of hospitalists report taking call, they carry the heaviest burden. On average, they take 2.1 call days per week (that’s once every 3.3 days), and two-thirds of those are in-hospital.
Nephrologists: 100% of Physicians Take Call, 1.6 Days per Week
With so few specialists in most hospitals, nephrologists are almost always on rotation. Every physician in our dataset reported taking call, averaging 1.6 days per week.
Infectious Disease Physicians: 90% Take Call, Nearly Every Other Day
Infectious Disease physicians also rank near the top, with 90% taking call at an average of 1.7 days per week. Nearly half of these are in-hospital, leaving little flexibility.
OB/GYN Physicians and Surgeons: 94% of Physicians on Call
Call is essentially universal for OB/GYN and Surgery. OB/GYNs average 1.4 call days per week (45% in-hospital), while Surgeons average 1.8 days per week (18% in-hospital). Both groups face unpredictable hours and urgent cases that require them on-site.
Anesthesiologists: 88% Take Call, 53% In-Hospital
Anesthesiologists report 1.2 call days per week, but the burden is magnified by the fact that more than half of these shifts require being in the in-hospita.
Specialties with Lighter Call:
Dermatology, Family Medicine, Urgent Care and Preventive Medicine fall on the other end of the spectrum, with much lighter demands:
- Dermatologists: 50% take call, averaging 1.4 days per week
- Family Medicine Physicians: 72% take call, averaging 1.3 days per week
- Urgent Care Physicians: 44% take call, averaging 0.9 days per week
- Preventive Medicine Physicians: Just 15% take call, averaging 1.5 days per week, all from home
Call is Ubiquitous, But How Often Is It Paid?
The data above shows just how demanding call schedules can be. In fact, 14% of physicians report a 1:3 or heavier rotation, meaning they’re on call at least every third night or more. For many, this is the single biggest driver of stress in practice.
Compensation for call can get complicated quickly. The norms vary by specialty, with payment structures varying widely - some employers may pay by the hour, while others pay by the night or by the shift. Still other physicians may get compensated for call based on a differential relative to their standard salary, or may have unpaid call written into their contracts.
We’ll unpack these models in detail and what “fair” looks like in next week’s post.p
A Case Study: Negotiating Call Coverage
In a recent contract review that Dennis negotiated for one of their physician clients, the hospital included only a vague clause: “call coverage will be assigned by Employer.” The administrator explained that the hospital “needed flexibility because it’s a business.” This was a classic case of hospitalsplaining - framing the physician’s concerns as secondary to organizational needs.
We raised three reasonable requests:
- Equitable distribution among all eligible providers.
- Limits on frequency, proposing a 1:5 rotation.
- Compensation for excessive call, pegged to market benchmarks
By citing benchmarks for what reasonable call looks like, we achieved meaningful changes: a cap on call days and pay for excess coverage. It wasn’t perfect, but it was far better than unlimited, unpaid call.
Based on our experience helping thousands of physicians negotiate their contracts over the past 40 years, here are some lessons physicians can apply while negotiating call requirements:
- Use benchmark data: Cite survey norms from Marit's physician salaries, MGMA, or any other sources you have access to. For example, hospitalists average 2.1 days per week with 67% in-hospital, while OB/GYNs average 1.4 days with 45% in-hospital.
- Stay professional and emphasize patient care: Frame limits not as perks but as safety measures. Burnout harms patient care. Reasonable call preserves quality outcomes for everyone.
- Negotiate creative compromises: Explore tiered models (baseline coverage plus paid excess), weekend stipends, or caps on frequency. Unlike salary, call compensation structures vary dramatically across practices.
- Bring in experienced support: This is a nuanced topic, and a physician contract attorney can help anchor requests in enforceable terms and avoid vague, one-sided clauses.
PS: For practical advice on Contract Review services, the terms you can negotiate, and whether they are worth the investment, see our deep-dive on Physician Contract survey results here
Final Thoughts
Call is a reality of medicine - patients need care at night, on weekends, and on holidays. But it doesn’t need to be unlimited, uncompensated, or unsafe. We hope this post helps provide some guidelines on how to turn unreasonable call demands into a manageable, and ideally compensated, part of your career.
Next week, we'll walk through a deep-dive on call compensation benchmarks.
About the Data & Methodology
Marit's Data is different. It is -
Unique - since it captures the compensation data along with all the details that matter - bonuses, shifts, scheduls, benefits, and more
Comprehensive - Across all specialties and Professions (Physicians & APPs), Employer Types (large and small, including Self-employed, Academic & Non Academic), Job Types (Full Time, Part Time, PRNs and Locums) and Employment Types (W-2, 1099, K-1)
Current - Unlike other benchmarks that only update their data once a year, all salaries reflect the clinician’s current compensation, and all averages are updated in real-time as new salaries are added
All data in this report comes from anonymized salary contributions on Marit, as of Aug 27, 2025. Only verified salary reports approved by our moderation team are included.
Feedback?
If you have any suggestions or requests for customized analysis or topics of research - we'd love to hear from you.
Dennis Hursh & Rob Anderson, MD
About the Authors
Dennis Hursh is a veteran physician’s attorney with over 40 years of experience in health law. He is founder of Physician Agreements Health Law, which offers a fixed fee review of physician employment agreements to protect physicians in one of the biggest transactions of their careers. He can also be reached on LinkedIn.
Dennis is a frequent lecturer on physician contracts to residency and fellowship programs and has spoken at events sponsored by numerous health systems and physician organizations, including the American Osteopathic Association, the White Coat Investor, the American Health Law Association, the American College of Rheumatology, and the American Podiatry Association.
Dennis has authored several published articles on physician contractual matters on forums such as KevinMD and Medscape. He is also the author of The Final Hurdle – A Physicians’ Guide to Negotiating a Fair Employment Agreement, the go-to resource for physician contract negotiation.
Rob Anderson, MD, is a practicing anesthesiologist at NAPA North American Partners, based out of Richmond, Virginia, and the co-founder of Marit Health.